
1VES Business School, Mumbai, Maharashtra, India
Creative Commons Non Commercial CC BY-NC: This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 License (http://www. creativecommons.org/licenses/by-nc/4.0/) which permits non-Commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
The global tobacco pandemic continues to cause enormous health burden and fatality, especially in the low and middle-income countries (LMICs), in spite of continuing efforts under the umbrella of FCTC. India, representing a complex pattern of tobacco use, both in smoking and smokeless forms, remains the second largest tobacco-using country. This study was designed to understand the impact of COVID-19 pandemic and associated restrictive measures on all groups of tobacco users and the impact on the users of e-cigarettes (EC), as a result of imposition of ban. A well-designed, online or CATI interview-based survey was conducted in eight large metropolitan cities of India on 3005 samples (smoking tobacco [ST]: 1,193; smokeless tobacco [SLT]: 966; and EC: 846). The study finds all groups were affected albeit differently
The COVID-19 crisis affected all tobacco user segments positively as well as negatively. EC users, unless supported appropriately, were likely to revert to tobacco use after having quit it successfully.
Tobacco, smoking tobacco, smokeless tobacco, e-cigarette, COVID-19, EC ban, tobacco cessation, India
Introduction
India has been among the leading member states of the World Health Organization (WHO) to adopt and ratify the Framework Convention on Tobacco Control (FCTC), which was negotiated in 2003 as a comprehensive public health response to the global tobacco pandemic (Framework Convention Alliance [FCA], 2020). The provisions of the FCTC were immediately given a legislative frame in India by enacting the Cigarette and Other Tobacco Products Act (COTPA) on 18 May 2003 (Ministry of Health and Family Welfare [MOHFW], 2003). Under this legislation and other related provisions, the plan of action formulated by the MOHFW, Government of India (GOI), aimed at reducing tobacco prevalence by 15% at the end of 2020 and by 30% by the year 2025 (MOHFW, 2018b). Yet, today, after over one-and-a-half decades, India remains the third largest producer and the second largest consumer of tobacco in the world. One of the main reasons attributable to the continuing high prevalence of tobacco burden in India is the diverse ways in which tobacco is manufactured, marketed and consumed. The latest Global Adult Tobacco Survey (GATS) report shows that India had 267 million adults using some form of tobacco, either smoking tobacco (ST) or smokeless tobacco (SLT), accounting for about 12% of the entire global tobacco consumption (MOHFW, 2018a). The Indian tobacco landscape included 199.4 million SLT users (masticators) and 99.5 million ST users (smokers), which was 28.6% of the entire ~15-year age group population comprising 42.4% men and 14.2% women (MOHFW, 2018a; Singh, 2020). While the prevalence of ST is seen in around 10.7% of Indian adults, it was estimated to be at least two-fold more for SLT (approximately 21.4%). In addition, it was also estimated that~30.2% of Indian adults were exposed to second-hand smoke in indoor workplaces, ~7.4% in restaurants and ~13.3% in public transportation (MOHFW, 2018a), further increasing the tobacco-related health burden. This acquired and avoidable lifestyle factor directly contributed to >1 million deaths every year in India, which is equivalent to ~3,500 deaths per day (Sinha et al 2014), significantly more (about 3½ times) than the real-time Indian mortality from the current COVID-19 pandemic (MOHFW, 2020). Nearly half of the deaths due to use of different forms of tobacco are attributable to cardiovascular diseases (CVD) and are primarily seen among the people of 30–59 years age group (WHO, 2018). Among current smokers, life expectancy is expected to contract by about 11 years for women and by about 12 years for men, compared to never-smokers (Jha et al, 2013). Tobacco consumption, primarily SLT, is also directly attributed to nearly 80% of all oral cancers as well as about 45% of all cancers among men and 17% among women, in India (International Agency for Research on Cancer [IARC], 2004; National Cancer Registry Programme [NCRP], 2013).
The rainbow spectrum of tobacco consumption in India has sustained primarily due to the availability of a variety of relatively inexpensive tobacco products. The range of ST products available in India includes indigenous, home-based, hand- rolled or small factory-manufactured products such as bidi, chillum and hookah, among others, besides the factory-made, different types and sizes of cigarettes. Similarly, SLT products include betel quid with tobacco, khaini, gutkha, zard, and paan masala, among about 40 other variety of products widely available in convenient small pouches to cheaper large packings. This wide range of products and practices combined with sociocultural and economic realities of India make tobacco control efforts complex and highly challenging, explaining, at least in part, the reasons for the poor tobacco control outcome (Farsalinos, Russel, et al., 2019). Under the provisions of COTPA (HOHFW, 2003), various agencies of the GOI responsible for tobacco control (Rao & Chaturvedi, 2010), have been applying standard measures, such as counselling with or without nicotine replacement therapies (NRTs), taxation on products, statutory health warnings on packings, advertisement bans, smoking or chewing tobacco prohibitions in healthcare establishments and educational institutions, and no smoking in public places, among others. Nonetheless, the outcome of the efforts has been anything but below expectations not only in India but also largely across the spectrum of the low and middle-income countries (LMICs). It is reported that in LMICs there has been an increase of 33 million tobacco users in the period between 2010 and 2015 (Action on Smoking and Health [ASH], 2019). In sharp contrast, during the same period, high-income countries (HICs) recorded positive impact of tobacco control measures with reduction of tobacco users by an estimated 62 million (ASH, 2019; Pierce et al, 1998).
One of the many possible reasons for the relative success of tobacco control in HICs is seen to be the availability of harm-reduced products (HRPs) among the other NRT options for those who wish to quit tobacco. Among various HRPs, electronic cigarette (EC) of different kinds has been the front-runner. EC is regarded as a convenient electronic device to meet the nicotine demand of a tobacco user. An EC is made up of a sequentially interconnected air inlet, an atomiser, an aerosol passage, and a mouthpiece with an atomiser and liquid supply containing pharmaceutical-grade nicotine dissolved in propylene glycol or vegetable glycerine with or without different flavouring agents (Grana et al., 2014; Public Health England [PHE], 2015; Royal College of Physicians [RCP], 2016). Though not absolutely safe, EC is devoid of almost all major toxicants and carcinogens typically found in ST or SLT preparations, except nicotine in equivalent quantity (Das et al., 2019; Farsalinos, Russel et al., 2019). Hence, EC, an HRP, is reported to be 95% less harmful than ST and is considered as a more pleasant alternative to the existing NRTs (PHE, 2015). Today, an estimated 400 different brands of EC are available along with multitude of e-liquids, including flavoured ones (Bhatnagar et al, 2014). One recent study from India on EC found that it was an effective NRT for both ST and SLT users, successfully helping them in quitting tobacco after shifting to EC. The users also reported some health benefits with minimal side effects (Sharan et al, 2020). However, Chakma and associates from the Indian Council of Medical Research (ICMR)—the apex body in India for the formulation, coordination and promotion of biomedical research— published a white paper in 2019 and recommended a complete ban on EC in India (Chakma et al., 2019). Though criticised by global scientists for cherry- picking favourable research publications and ignoring credible but unfavourable scientific reports in drawing its conclusion in this white paper (Farsalinos, Ambekar, et al., 2019), the GOI accepted the recommendations of the white paper and promulgated a complete ban on EC in India with effect from September 2019 (MOHFW, 2019).
Another pandemic, COVID-19, gripped the world in a most unprecedented way in the first few months of the year 2020, which still prevails across different geographical barriers (MOHFW, 2020; WHO, 2020). It has tremendously affected all aspects of lives, livelihoods and living across the globe due to the lockdowns and other restrictive measures to control the spread of the virus. Consequences of such measures have been widespread, resulting in closure of businesses, collapse of supply chains, economic slowdowns, and strained health and other medical services that could potentially adversely affect tobacco users both psychologically and physiologically as many of them could have been deprived of their usual nicotine requirement.
Keeping the existing magnitude and complexity of Indian tobacco landscape and its massive national health burden in mind, which might have got further compounded due to the COVID-19 pandemic and the related lockdown and restrictive measures during the current period, this study was designed to primarily capture and analyse the impact of the pandemic on ST and SLT users holistically. Since EC, a widely accepted safer substitute for nicotine replacement, was also banned in India just about six months prior to the onset of the COVID-19 pandemic, we have additionally tried to capture that impact as well on the EC users who were facing a dual situation—the COVID-19 pandemic and the EC ban. Hence, the primary objective of this study was to understand and analyse the similarities and differences in the impacts of the COVID-19 pandemic on the three exclusive groups of people habitually using ST, SLT (including pharmaceutical products such as nicotine gums, patches and lozenges) and EC in India. An additional objective was to also map the impact of the ban of EC in India currently in effect during this COVID-19 pandemic period. The null hypothesis formulated for the study was as follows: the COVID-19 pandemic effected tobacco (ST and SLT) as well as EC using population groups equally in India.
Methodology
A pan-India, cross sectional survey-based study, designed on a random, convenience sampling model, was conducted on adult subjects aged 18 years and above, the inclusion criteria being current or former tobacco users of any form of tobacco/ nicotine—ST and/or SLT, or an EC user. Eight largest metropolitan Indian cities (Ahmedabad, Bengaluru, Chennai, Delhi, Hyderabad, Kolkata, Mumbai and Pune) were chosen for the survey-based study. A sample size of 3,000 was targeted in order to increase the power to conduct analysis of different subgroups (e.g., ST, SLT, EC, gender, prevalence, health, etc.). A structured format of survey in English was developed for the study, which was tested in two successive batches to minimise potential misunderstandings and conflicts in the given responses. A final questionnaire was developed based on the test and was implemented utilising the online survey platform the Survey Monkey. The questionnaire consisted of eight sections covering the socio-demographic profiles, history of exposure to tobacco, usage patterns of ST and SLT to understand their prevailing status, impact of COVID-19 on tobacco usage patterns, usage patterns of EC, and the impact of the COVID-19 pandemic and the EC ban on the status of EC use.
The survey questionnaire was uploaded on the Survey Monkey portal and the link was spread randomly across potential subjects in the eight selected metropolitan cities. The survey was conducted either online (self-administered) or in computer-assisted telephonic interview (CATI) mode, where needed. In all cases, a unique respondent ID was maintained to facilitate random validation of responses. We followed ESOMAR guidelines for fieldwork for the study (International Chamber of Commerce [ICC] & ESOMAR, 2016). Survey results were collated in Microsoft Excel format for further analysis as well as to produce certain pre-designed dashboards to validate the analysis.
Statistical analysis: Statistical analysis was conducted using SPSS Statistics package (v 20.0). All categorical values have been reported as percentages. Descriptive statistics was applied to measure the differences between socio- demographic variables and tobacco (ST and SLT) or EC consumptions using Pearson Chi-square test at a significance level of p < .05.
Results
Demographics
A total of 3,489 subjects from the eight target cities in India returned the survey. Of them, 3,005 responses were selected for further analysis based on the inclusion and exclusion criteria. This final dataset consisted of 39.7% (1,193) ST users or smokers; 32.1% (966) SLT, including pharmaceutical tobacco products such as nicotine gums, patches and lozenges users or masticators; and 28.2% (846) EC users or vapers (Figure 1).
Participants belonged to almost all states and union territories (UTs) of India by their state or UT of birth (domicile). However, more than 50% of them belonged to four large states, that is, Maharashtra (19.7%; 593), Gujarat (12.9%; 389), Karnataka (11.0%; 331) and West Bengal (9.7%; 291), while about six small states and UTs returned less than four responses each. While Maharashtra topped the count among smokers and masticators, Gujarat topped among vapers.
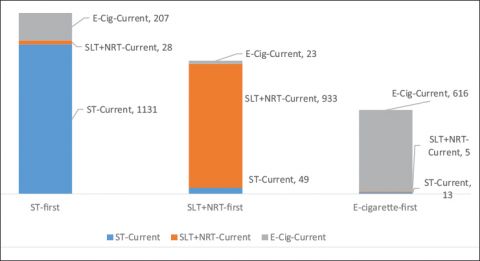
Route of first exposure to nicotine: Nearly half of the subjects (45.5%; 1,366/3,005) had the first exposure to nicotine via smoking while about one-third (33.4%; 1,005/3,005) through SLT, together making tobacco the major initiator of nicotine exposure for the Indian population (78.9%; 2,371/3,005). Currently, 92.8% (933/1005) of the subjects whose first exposure to nicotine was through SLT products continue with SLT as compared to 82.8% (1,131/1,366) in the ST group. EC was found to be the route of first exposure to nicotine for 21.1% (634/3,005) of the population, almost all of which continue to use EC (97.2%; 616/634) currently. Overall, 89.2% (2,680/3,005) of the subjects continued using the first product they used for nicotine exposure. Among the remaining 10.8% (325/3005), who shifted to other products different from first exposure, 72.3%.
Figure 1. Distribution of Study Sample.
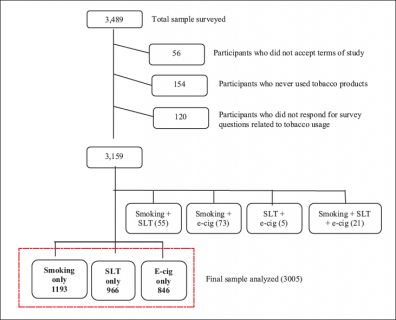
Note: SLT = Smokeless tobacco users; e-cig = Electronic cigarettes users.
(235/325) were smokers. Among smokers, 85% (1,020/1,193) were cigarette smokers, 72% (693/966) were masticators using gutkha and 42.6% (360/846) were vapers using pods (open system EC; Figure 2).
Tobacco usage pattern: Majority of the subjects (38.5% of smokers, 45% of masticators and 59% of vapers) have been using the products since 1–5 years and were currently using them on a daily basis. Most of the ST (65%; 777/1,193) and SLT (65%; 623/966) users took their first dose of the product on a regular day 30 minutes or later after waking up in the morning. Both user groups felt the strongest urge of the product in the mornings than the rest of the day, with nearly equal levels of restlessness (Χ2; p = .89) in places or situations where use of tobacco products was forbidden. While the smokers did not feel like smoking when unwell, masticators continued using SLTs (Χ2; p < .0001). More than 60% of both ST and SLT users self-reported that they were addicted to it (Χ2; p = .15). Among smokers, more than half (56%) felt that menthol cigarettes were safer than non- menthol cigarettes and 67% of masticators lived with the fear of getting oral or other cancers (Table 1).
EC usage pattern: Majority (59.0%; 499/846) of vapers had been using EC for the last one to five years at a frequency of twice/thrice (33.0%; 279) or less (23.9%; 202) a week. While a fourth (25.1%; 367) of them started using it because they felt EC was less toxic than tobacco, about an equal number of users.
Table 1. Usage Patterns of Tobacco Among Smokers (ST Group) and Smokeless Tobacco (SLT Group) Users.
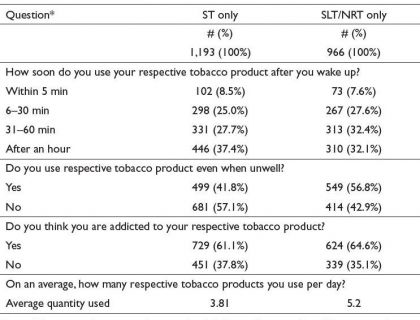
Note: *Non-responders are not shown in the table. Ranged between 13 and16 among smokers and three non-responders among SLT/NRT group.
Figure 2. Tobacco Product Currently in Use Against the First Ever Product Used (N = 3,005).
(23.7%; 347) had the moral satisfaction of consuming something smokeless without inconveniencing others. EC was introduced to majority of vapers by friends (peers; 40.4%; 342) or by online sale portals (27.4%; 232). The most commonly used nicotine strength among vapers was in the range of 4–12 mg (63.5%; 627). A large number of users liked free-base nicotine (43.4%; 413), while some preferred nicotine salts (31.7%; 301). About one-fourth (24.9%; 237) of vapers were using EC without nicotine (Table 2).
Table 2. Usage Patterns of EC Among Vapers.
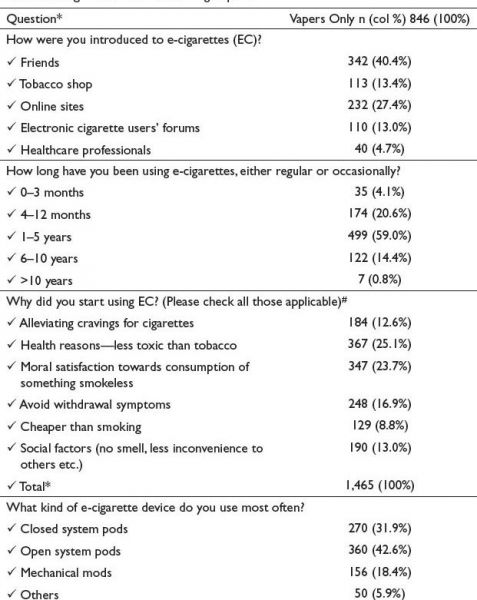
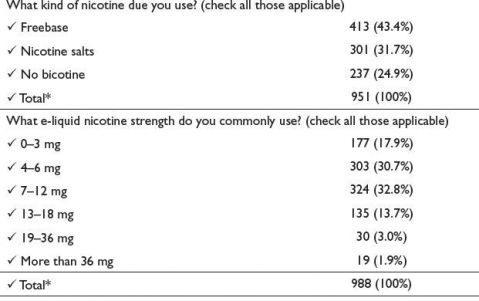
Notes: *Non-responders are not shown in the table. Ranged between 9 and 10 for various questions.
#Total responses for few questions are more than the sample size as multiple responses were allowed.
Influence of EC on tobacco cessation and health of users: Majority of EC users (35.9%; 304) took 3–6 months for shifting from smoking to vaping while some (27.7%; 234) did it in under three months. Due to switching to EC, approximately 44.4% (376) smokers could completely quit smoking and 71.6% (606) could completely quit chewing for variable periods. About one-third smokers and a significantly large, two-thirds, of masticators, on the other hand, did not experience such benefits . It was interesting to note that a majority (85.2%; 721/846) of vapers were clear that EC vaping was a low-risk alternative to smoking or masticating but was itself not totally harmless. Nearly half (48.5%; 410/846) of the respondents felt better in their overall status of health since they started using EC, while 39.7% (336/846) felt no significant change and 8% (68/846) felt that their health condition worsened. On the other hand, about one- fifth of the vapers (21.4%; 181/846) reported worsening of smell, and a smaller fraction, 12.1% (103/846), worsening of breath. Major side-effects self-perceived by the vapers were chest pain (18%), headache (16.2%), abdominal pain (15.1%) and throat irritation (15.1%), which together contributed to nearly 65% of all complaints.
Effects of CoViD-19 pandemic related restrictive measures on smokers, masticators and vapers: Over three-fourth of smokers (75.9%) and two-third of masticators (66%) as well as a large majority of vapers (75.2%) reported an overall significant impact of COVID-19 pandemic on their respective consumption patterns (Χ2; p < .05). Compared to the pre-COVID-19 pandemic period, consumption of tobacco products on a daily basis reduced by 44.3% (506 to 282 users) among smokers, by 27.3% (594 to 432) among masticators and by 20.9% (182 to 144) among vapers during the pandemic. Weekend consumptions declined marginally by 25.6%, 7.1% and 6.6%, respectively. However, there was a significant rise in tobacco consumption during stress of any kind on the user, with masticators recording 171.7% and smokers recording 101.4% increase in consumption. In contrast, under a comparable situation, the increase in vaping was found to be only 36.2% under stressful situations. A social factor, such as the company of friends (peers), affected tobacco and EC usage patterns differently. While it positively influenced smoking by13.9% and masticating by 16.0%, it negatively impacted vaping by 9.1% . On the other hand, another factor, fear of seriously falling ill during the COVID-19 pandemic, affected all three groups almost equally (28.2%, 35.9% and 28.5%, respectively, for ST, SLT and EC groups). Though nearly a fourth of all user groups felt restless during the COVID- 19-related lockdown and restrictions, they also saw it as an opportunity to quit tobacco completely. This was found to be highest among vapers (35.5%). Fewer smokers (22.7%) and even less masticators (12.7%) felt the same (Χ2 p < .05). All three user groups tried procuring respective products from friends, neighbours and street vendors, braving the risk of contracting COVID-19 infection when they were out of supply. This, however, also reinforced each user group’s desire of quitting nearly equally (57.1% among smokers, 53.6% among masticators and 60.6% among vapers; Χ2 p < .05) during the lockdown. Over one-third (38.7%) of smokers as well as vapers and slightly less (31.6%) of masticators made more than two attempts to quit, while a much larger number of users in each group (70.2% among smokers, 65.8% among masticators and 73.8% among vapers) made at least one attempt to quit during the lockdown period. Most users in all three groups considered talking to a doctor, nurse or counsellor and/or attending a class or group programme for help in their attempt to quit. Though there was no significant difference in opinion among tobacco users about the affordability of pharmaceutical cession products (Χ2; p = .051), the smokers felt that NRTs could help in quitting if they were cheaper (Χ2; p < .05). More than half of vapers had stocked up e-liquids, which could cater to their needs for a few months . When analysed for the factors influencing the process of quitting, the order of priority was cost, availability, harmful effects, convenience and social response across all the users.
Effects of EC ban on the vapers: More than 90% (763/864) of the respondents in this cohort were aware of the ban on EC imposed by the GOI, and approximately 60% (504/864) felt the ban was okay. Nearly two-third of subjects (68.9%; 583/846) were sure about EC being less harmful than other forms of tobacco wherein the SLT products were the most harmful . Two-third (77.3%; 654/846) of subjects were afraid that the EC ban will push them back to smoking again. Among them, while 44.9% (789) favoured switching to pharmaceutical alternatives followed by SLT and ST, 25.2% (442) opted for procurement through online resources, friends abroad or the black market, and 29.9% (525) preferred taking up meditation and/or seeking support of friends and family members to reduce or quit EC. While the respondents felt that the justifications given for banning EC were largely okay about its adverse effects on foetal development and pregnancy, they found others only partially correct (e.g., respiratory, cardiovascular and neurological disorders and carcinogenicity). About 45.2% (382) of vapers felt that the ban was not justified with the given reasons, while the remaining majority was neutral on the claimed effects of EC on DNA damage, and cellular, molecular and immunological toxicities as the reasons for banning EC in India . At the same time, 49.2% (416) respondents felt that the ban had some social merit and has health benefits, and around 52.6% (445) felt that the ban would help them in quitting tobacco (Table 3).
Table 3. Impact of EC Ban on Vapers in India.
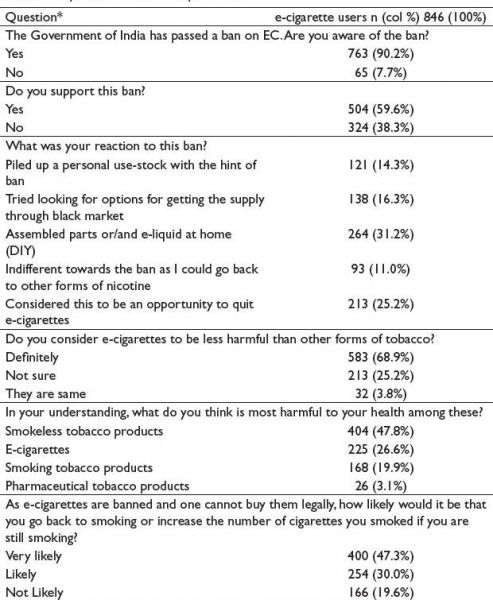
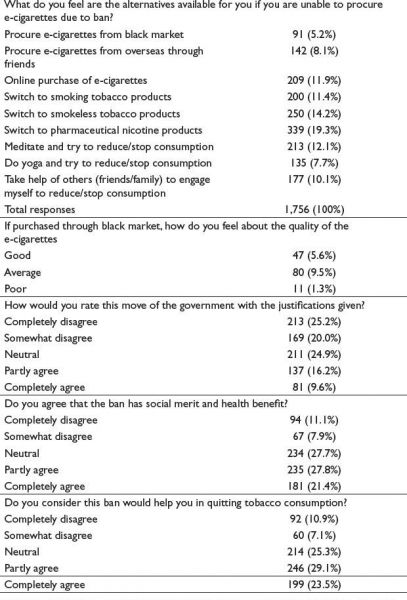
Note: *Non-responders are not shown in the table. Non-responders ranged between 17 and 35 years in different questions.
Discussion
India continues to be a complex public health challenge due to the diverse ways in which tobacco products are manufactured, marketed and consumed, thus encouraging a large number of people to indulge in use of a variety of tobacco products (Shah et al, 2018). There are conclusive evidences of this habit resulting in disease, disability and death. (Mishra et al., 2012). The challenge is severe and all-encompassing, covering issues of lives and health, livelihood and economy, and direct and indirect impact on national productivity, causing a multifaceted problem with biomedical, economic and geopolitical impacts (Mohan et al., 2018). Despite all efforts to contain this tobacco pandemic since the adoption of FCTC and the consequent enactment of COPTA in 2003 in India (MOHFW, 2003), tobacco control appears way behind the set targets of the GOI’s plan to reduce the national tobacco burden by 15% by the end of the current year of 2020 and, further, by 30% by the year 2025 (MOHFW, 2018b). It becomes further evident when we consider the prevalence of tobacco usage data for India in the GATS-2 report covering the 2016–2017 period (MOHFW, 2018a). The data shows that India continues to be home to over 267 million tobacco users, making it the second largest tobacco-consuming population in the world where over 20% of the entire population and 48% if men used tobacco in one or other form. Over the period of about eight years since GATS-1, the absolute tobacco usage in India decreased only by 6% (from 34.6% to 28.6%) and the prevalence among minors (15–17 years) decreased from 10% to 4%, with the age of initiation increasing by an average of one year for smokers (from ~17.9–~18.9 years). While these are positive correlates, India also recorded the second lowest quit rate among the GATS-2 countries despite the high prevalence of public knowledge about the grave health consequences of smoking tobacco and/or chewing SLT. GATS-2 data also showed that only about 55% of smokers and 50% of masticators ever thought of or intended to quit, with poor to very poor success rates. The use of behavioural and pharmacological interventions towards cessation approach has been found to have a positive impact on tobacco cessation outcomes (Nethan et al., 2018). Recognising this, the India Tobacco Cessation Centres (TCC) were mandated to provide both behavioural and pharmacotherapy interventions. However, it has been observed that a very limited number of tobacco users accessed these clinics with very limited cessation outcome (Thankappan, 2014), raising serious questions on the effectivity of TCCs in the field.
A major concern is over the evidence coming from medical, social and behavioural sciences exhibiting 58 million women and young girls as SLT users. India currently has 58 million women users of SLT products and over half of them do not desire to quit (Singh et al., 2020). And the worrying reality is that smoking is predicted to rise further in LMICs, which includes India (Lancet Editorial, 2018; Roy et al, 2017; WHO, 2015).
India faced, along with rest of the world, an unprecedented situation with the advent of the COVID-19 pandemic since March 2020, which is still ongoing (Li et al., 2020; Pal & Yadav, 2020; Wu et al., 2020). This pandemic necessitated impositions of national lockdowns and severe restrictions across India. All efforts to contain the COVID-19 pandemic have been, at best, marginally successful till now. This second pandemic related to COVID-19 has also affected the lives and livelihoods of people in an unforeseen way, and perhaps as intensely as the tobacco pandemic did in the beginning of the millennium and continues to do so to its users. Therefore, we designed and conducted this study, which we believe is first of its kind in India, to primarily capture and analyse the impact of the COVID- 19 pandemic on tobacco users (both combustible tobacco smokers and smokeless tobacco masticators) holistically in a pan-India coverage mode as far as practicable. In an effort to reduce the global tobacco health burden, technologies have been in development in the last about a decade or so to deliver nicotine in a relatively safe form, minimally contaminated with tobacco-specific toxicants and carcinogens, to a person dependent on tobacco for the nicotine supply. Such technologies are increasingly becoming popular additional avenues of meeting the nicotine demand of a tobacco user in several HICs where it is also helping a user in their tobacco cessation effort (ASH, 2019; Das et al., 2019; RCP, 2016; Sharan et al., 2020). Today, various electronic nicotine delivery systems are available, among which EC are the oldest and perhaps most widely used in several countries. GATS-2 estimated that about 0.02% or approximately 0.19 million Indians aged 15 years or above used EC at that time (MOHFW, 2018a). Though under intense debate over its safety and efficacy concerns, GOI banned it a few months earlier than the advent of the COVID-19 pandemic (MOHFW, 2019). Since India had small but sizeable number of EC users, through this survey-based study, we attempted to monitor the state of the vapers now under dual restrictions—first, from the imposed ban, and second, due to the COVID-19 pandemic.
It was interesting to see that a significant majority in all three user groups were impacted differently by the lockdown and restrictions imposed due to the prevailing COVID-19 pandemic. Tobacco users had an overall higher impact than the EC group. Compared to the pre-COVID-19 period, the daily consumption was reported to reduce maximally among smokers (44.3%), while it was a bit less for masticators (27.3%), reaching a minimum (20.9%) among vapers, which declined further variably during the weekends. It was intriguing to note that the maximum decline during the COVID-19 pandemic and lockdown restriction was reported by smokers (ST group) compared to a marginal decline reported by masticators (SLT group) as well as vapers (EC group), suggesting possibly that the indoor stay and/or the presence of other members of the household or both might have acted as a stronger deterrent to smoking only and not to masticating or vaping. In contrast, under stress situations, both tobacco user groups reported a huge surge in their consumption patterns (101.4% and 171.7% for ST and SLT groups, respectively) as compared to a significantly low increase in the vaper group (36.2%), even though all three user groups reported almost equal (28.2%, 35.9% and 28.5% for ST, SLT and EC users, respectively) fear of contracting COVID-19 infection during the pandemic and the lockdown .The fear of its unavailability due to lockdown made them pile up stock and considering it to be their primary mechanism in controlling stress and anxiety made them consume more (Report of National Cancer Registry Programme, 2020; Yach, 2020). Does it indicate that tobacco use makes people more stress-prone in comparison to EC use is a proposition that should be investigated further.
It was heartening to note that the restrictions and the lockdown adversely affected the supply of all tobacco products as also the components of EC, making all three user groups think almost equally resolute to use the opportunity to quit tobacco. This is in contrast to a study conducted in Italy where the majority of exclusive cigarette smokers have considered quitting while very few exclusive EC users have considered quitting (Caponnetto et al., 2020.) However, we recorded a positive outcome of the COVID-19 pandemic and its associated lockdown and restrictions in terms of tobacco cessation, which made 57.1% smokers, 53.6% masticators and 60.6% vapers think of quitting and approximately two-third (70.2%, 65.8% and 73.8%, respectively) making at least one, and about one-third (38.7%, 31.6% and 38.7%, respectively) making two, attempts to quit during the period of our study. It is apparent that the desire as well as the attempts to quit are influenced not only by the addictive potential of a product but also by several other contributing factors (e.g., cost, availability, health impact, etc.), as also noted in several previous studies (Copeland & Brandon., 2000; Hymowitz et al., 1997; Maddux & Roggers 1983; McCaul et al 2006; Orleans et al, 1994; Romer & Jameson, 2001). This is reflected in the marginally stronger motivation noted among vapers to take the lockdown and restrictions as opportunities to quit in relation to tobacco users, wherein the motivation level was found to be higher among smokers and least among masticators.
The cohort of vapers, quite well aware of the ban imposed on EC in India about six months before the COVID-19 pandemic, reacted in a mixed way to the forced ban . More than 50% felt that the ban was okay in general and may have some social merits. Nearly two-third of users knew that EC was a safer option than tobacco products and expressed fear that the EC ban would push them to tobacco use again, which most of them did not desire . This clearly shows the maturity of EC users who seem to be reasonably well aware of the science behind the health implications of EC. This study finds that almost 49% of vapers feeling that with vaping they consumed something that is not only smokeless but also less toxic. This motivation may be an important contributing factor for their continuing with EC.
Limitations
A limitation of this study is that it was designed on convenience sampling; hence, it cannot assure representing the entire Indian population. Additionally as the study wanted to understand the impact of lockdowns, hence, it had to be completed within a short time-frame. Also being a cross-sectional study, it is unable to confirm the causal relationship. The impact study of COVID-19 on tobacco consumption should be expanded to tier-II cities and rural India too.
Conclusions
The primary aim of the study was to holistically capture a pan-India impression of the COVID-19 pandemic on both ST and SLT users in India. A small fraction of the Indian population has been using ECs, believed to be a technology-driven nicotine delivery device and considered a reduced-harm product with tobacco cessation potential, before it was banned in September 2019. The study finds revealing patterns of ST, SLT and EC usage as well as the effectivity of EC as a technology driven source of meeting the demand of nicotine of typical tobacco users in the Indian populations that can be potentially useful in the ongoing efforts to control the tobacco pandemic in India and help realise its committed goals towards reducing the tobacco burden. We find that the COVID-19 induced lockdown and restrictions affected both tobacco user segments and EC user groups. The COVID-19 pandemic was also seen by a large segment of all three user groups as an opportunity to quit tobacco. On the other hand, vapers, who had successfully quit combustible as well as smokeless tobacco with its help, were likely to revert to tobacco products unless supported appropriately and adequately. Though the EC cohort did not agree with the justifications for imposing the ban, they also felt it had social merit and health benefits and, thus, were willing to use it as an opportunity to quit tobacco using lifestyle factors such as meditation and yoga; consultation with doctors, nurses and counsellors; and classes or programmes tailored towards cessation.
Acknowledgements
The authors extend their thanks to Dr Chakrapani Chatla (public health specialist, Hyderabad, India) for his support and review of data management and analysis. We extend our gratitude to Professor R. N. Sharan (Department of Biochemistry, North-Eastern Hill University, Shillong) for providing insightful feedback through review and editing. Special thanks to Mr Samrat Choudhury, director HRPR, for funding the research project. We thank all the respondents who agreed to give their response to make this study complete successfully.
Declaration of Competing Interests
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Financial support was provided for the completion of this research work by Harm Reduction Policy & Research (HRPR, Mumbai, India). The funding agency had no involvement in designing, collection, analysis and interpretation of data, or writing of report and decision to submit the research work for publication.
Action on Smoking and Health. (2019). Fact sheet: Tobacco and the developing world. https://ash.org.uk/uploads/Tobacco-Developing-World.pdf
Bhatnagar, A, Whitsel, L. P., Ribisl, K. M., Bullen, C., Chaloupka, F., Piano, M. R., Robertson, R. M., McAuley, T., Goff, D., Benowitz, N. American Heart Association Advocacy Coordinating Committee, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, & Council on Quality of Care and Outcomes Research. (2014). Electronic cigarettes: A policy statement from the American Heart Association. Circulation, 130, 1418–1436. https://doi.org/10.1161/CIR.0000000000000107
Caponnetto, P., Inguscio, L., Saitta, C., Maglia, M., Benfatto, F., & Polosa, R. (2020). Smoking behavior and psychological dynamics during COVID-19 social distanc- ing and stay-at-home policies: A survey. Health Psychology Research, 8(1), 68–74. https://doi.org/10.4081/hpr.2020.9124
Chakma, K. J., Dhaliwal, R. S., & Mehrotra, R. (2019). White paper on electronic nicotine delivery system. Indian Council of Medical Research. https://doi.org/10.4103/ijmr. IJMR_957_19
Copeland, A. L., & Brandon, T. H. (2000). Testing the causal role of expectancies in smok- ing motivation and behavior. Addictive Behaviors, 25(3), 445–449. https://10.1016/ S0306-4603(99)00003-9
Das, S., Choudhury, Y., & Sharan, R. N. (2019). A systematic review and meta-analysis on the health and safety implications of Electronic Nicotine Delivery Systems. Indian Journal of Clinical Practice, 29(11), 1016–1026. https://ijcp.in/Pages/Post_Detail. aspx?wid=20305&A%20Systematic%20Review%20and%20Meta-analysis%20 on%20the%20Health%20and%20Safety%20Implications%20of%20ENDS
Farsalinos, Ks., Ambekar, A., & Polosa, R. (2019b). White Paper on electronic nicotine delivery systems by the Indian Council of Medical Research: A critical appraisal of the scientific evidence. Indian Journal of Clinical Practice, 30(3). https://ijcp.in/Admin/ CMS/PDF/03_Original%20Article_G02.pdf
Farsalinos, K., Russell, C., & Sharan, R. (2019). The prospects of e-cigarettes in India: Overview of evidence, opportunities and challenges based on experience in western countries. Indian Journal of Clinical Practice, 29(12), 1106–1120. https://ijcp.in/ Admin/CMS/PDF/Perspective.pdf
Framework Convention Alliance. (2020). Parties to the WHO FCTC (ratifications and accessions). https://www.fctc.org/parties-ratifications-and-accessions-latest/
Grana, R., Benowitz, N., & Glantz, S. A. (2014). E-cigarettes: A scientific review.
Circulation, 129(19). http://dx.doi.org/10.1161/CIRCULATIONAHA.114.007667 Hymowitz, N., Cummings, K. M., Hyland, A., Lynn, W. R., Pechacek, T. F., & Hartwell, T. D. (1997). Predictors of smoking cessation in a Cohort of adult smokers followed for five year. Tobacco Control, 6(Suppl. 2). https://doi.org/10.1136/tc.6.suppl_2.s57
International Chamber of Commerce. & ESOMAR. (2016). ICC/ESOMAR interna- tional code on market, opinion and social research and data analytics. International Chamber of Commerce. https://www.esomar.org/uploads/pdf/professional-standards/ ICCESOMAR_Code_English_.pdf
International Agency for Research on Cancer. (2004). Tobacco smoke and involuntary smoking (IARC Working Group on the Evaluation of Carcinogenic Risks to Humans). IARC Monographs on the Evaluation of Carcinogenic Risks to Humans (Vol. 83). IARC.
Jha, P., Ramasundarahettige, C., Landsman, V., Rostron, B., Thun, M., Anderson, R. N., McAfee, T. D., & Peto, R. (2013). 21st century hazards of smoking and benefits of cessation in the United States. New England Journal of Medicine, 368, 341–350. https://doi.org/10.1056/NEJMsa1211128
Lancet Editorial. (2018). Progress towards a tobacco-free world. Lancet, 392(10141), 1. https://doi.org/10.1016/S0140-6736(18)31482-X
Li, Q., Guan, X., Wu, P. et al. (2020). Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. New England Journal of Medicine, 382(13):1199–1207. doi:10.1056/NEJMoa2001316
Maddux, E. J., & &Rogers, W. R., (1983). Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. Journal of Experimental Social Psychology, 19(5), 469–479. https://doi.org10.1016/0022-1031(83)90023-9
McCaul, K. D., Hockemeyer, J. R., Johnson, R. J., Zetocha, K., Quinlan, K., & Glasgow, R. E. (2006). Motivation to quit using cigarettes: A review. Addictive Behaviors, 31(1), 42–56. https://doi.org/10.1016/j.addbeh.2005.04.004
Ministry of Health and Family Welfare. (2003). The Cigarettes and Other Tobacco Products (prohibition of advertisement and regulation of trade and commerce, pro- duction, supply and distribution) Act, 2003. An Act enacted by the Parliament of Republic of India by notification in the Official Gazette (Act 32 of 2003).
Ministry of Health and Family Welfare. (2018a). Global Adult Tobacco Survey GATS 2 India 2016–17. Tata Institute of Social Sciences and Ministry of Health and Family Welfare, Government of India.\
Ministry of Health and Family Welfare. (2018b). Report on Tobacco Control in India, 2004. Ministry of Health and Family Welfare, Government of India. http://www.who. int/fctc/reporting/Annex6_Report_on_Tobacco_Control_in_India_2004.pdf
Ministry of Health and Family Welfare. (2019). The Prohibition of Electronic Cigarettes (Production, Manufacture, Import, Export, Transport, Sale, Distribution, Storage and Advertisement) Bill, 2019. https://www.prsindia.org/billtrack/prohibition-electronic- cigarettes-production-manufacture-import-export-transport-sale-0
Ministry of Health and Family Welfare. (2020). COVID-19 INDIA. Ministry of Health and Family Welfare, Government of India. https://www.mohfw.gov.in/
Mishra, G. A., Pimple, S. A., & Shastri, S. S. (2012). An overview of the tobacco problem in India. Journal of Medical and Pediatric Oncology: Indian Journal of Medical and Pediatric Oncology, 33(3), 139–145. https://doi.org/10.4103/0971-5851.103139
Mohan, P., Lando, A. H., & Panneer, S. (2018) Assessment of tobacco consump- tion and control in India. Indian Journal of Clinical Medicine, 9, 1–8. https://doi. org/10.1177/1179916118759289
National Cancer Registry Programme. (2013). Consolidated Report of Hospital Based Cancer Registries 2007–2011. National Cancer Registry Programme, Indian Council of Medical Research.
National Cancer Registry Programme. (2020). Indian Council of Medical Research/ National Centre for Diseases Informatics and Research. https://ncdirindia.org/All_ Reports/Report_2020/Brf_2020/NCRPReport202_Brief_write_up.pdf
Nethan, S. T., Sinha, D. N., Chandan, K, Mehrotra, R. (2018). Smokeless tobacco cessa- tion interventions: A systematic review. Indian Journal of Medical Research, 148; 396–410. https://doi.org/10.4103/ijmr.IJMR_1983_17
Orleans, C. T., Jepson, C., Resch, N., & Rimer, K. B. (1994). Quitting motives and barriers among older smokers. The 1986 Adult use of tobacco survey revisited. Cancer, 74(7 Suppl.), 2055–2061. https://doi.org/10.1002/1097-0142(19941001)74:7+<2055:AID- CNCR2820741712>3.0.CO;2-Q
Pal, R., & Yadav, U. (2020). COVID-19 Pandemic in India: Present scenario and a steep climb ahead. Journal of Primary Care & Community Health, 11. https://doi. org/10.1177/2150132720939402
Pierce, J. P., Gilpin, E. A., Emery, S. L., White, M. M., Rosbrook, M., & Berry, C. (1998) Has the California tobacco control program reduced smoking? Journal of the American Medical Association, 280(10), 893–899. https://doi.org/10.1001/jama.280.10.893
Public Health England. (2015). E-cigarettes around 95% less harmful than tobacco esti- mates landmark review. https://www.gov.uk/government/news/e-cigarettes-around- 95-less-harmful-than-tobacco-estimates-landmark-review
Rao, V., & Chaturvedi, P. (2010). Tobacco and health in India. Indian Journal of Cancer, 47(5), 3–8. http://www.indianjcancer.com/text.asp?2010/47/5/3/64373
Royal College of Physicians. (2016). Nicotine without smoke: tobacco harm reduction. RCP report on e-cigarettes. https://ukctas.net/rcp.html#:~:text=The%20Royal%20 College%20of%20Physicians,are%20muc
Romer, D., & Jamieson, P. (2001). The role of perceived risk in starting and stopping smoking. In P. Slovic (Ed.), Smoking: Risk, perception, & policy (pp. 64–80). SAGE Publications. https://doi.org/10.4135/9781452232652.n4
Roy, A., Rawal, I., Jabbour, S., & Prabhakaran, D. (2017). Tobacco and cardiovascular disease: A summary of evidence. In D. Prabhakaranj, S. Anand, T. A., Gaziano, J. C. Mbanya, Y. Wu & R. Nugemt (Eds), Cardiovascular, respiratory, and related disor- ders (Vol. 5, 3rd ed.). https://doi.org/10.1596/978-1-4648-0518-9
Sharan, R. N., Chanu, T. M., Chakrabarty, T. K., & Farsalinos, K. (2020). Patterns of tobacco and e-cigarette use status in India: A cross-sectional survey of 3000 vapers in eight Indian cities. Harm Reduction Journal, 17, 21. https://doi.org/10.1186/s12954- 020-00362-7
Shah, S., Dave, B., Shah, R., Mehta, T. R., & Dave, R. (2018). Socioeconomic and cul- tural impact of tobacco in India. Journal of Family Medicine and Primary Care, 7(6), 1173–1176. https://doi.org/10.4103/jfmpc.jfmpc_36_18
Singh, S., Jain, P., Singh, P. K., Reddy, K. S., & Bhargava, B. (2020). White paper on smokeless tobacco & women’s health in India. Indian Journal of Medical Research, 151, 513–521. https://doi.org/10.4103/ijmr.IJMR_537_20
Sinha, D. N., Palipudi, K. M., Gupta, P. C., Singhal, S., Ramasundarahettige, C., Jha, P., Indrayan, A., Asma, S., & Vendhan, G. (2014). Smokeless tobacco use: A meta-anal- ysis of risk and attributable mortality estimates for India. Indian Journal of Cancer, 51(Suppl. 1), S73–S77. https://doi.org/10.4103/0019-509X.147477
Thankappan, K. R. (2014). Tobacco cessation in India: A priority health intervention. The Indian Journal of Medical Research, 139(4), 484–486.
World Health Organization. (2015). Cardiovascular diseases: Fact sheet. https://www. world-heart-federation.org/wp-content/uploads/2018/05/Factsheet-Tobacco-and- CVD_Healthcare-professionals-v2.1.pdf
World Health Organization. (2018). Factsheet 2018 India. https://apps.who.int/iris/bit- stream/handle/10665/272672/wntd_2018_india_fs.pdf?sequence=1
World Health Organization. (2020). Coronavirus disease 2019 (COVID-19) (Situation Report-40). https://www.who.int/docs/default-source/coronaviruse/situation-reports/ 20200229-sitrep-40-covid-19.pdf?sfvrsn=849d0665_2
Wu, J. T., Leung, K., & Leung, G.M. (2020). Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: Modelling study. Lancet, 395(10225), 689–697. https:doi.org/\:10.1016/ S0140-6736(20)30260-9
Yach, D. (2020, 9 September). Tobacco use patterns in five countries during the Covid-19 lockdown. Nicotine & Tobacco Research, 22, 1671–1672. https://doi.org/10.1093/ntr/ ntaa097